
Evidence-Based Population Health Improvement Plan
Hello to all of you. My name is (Student). I will be presenting an NURS FPX 6011 Assessment 2 Evidence Based Population Health Improvement Plan now to combat obesity in our neighborhood.
Creating strategies for improving general health, according to research, is essential for addressing complicated global health problems, including obesity. These plans provide municipalities the ability to strategically deploy funds and organize their activities according to the evaluation of health gaps and requirements. Strategies that are grounded on evidence also encourage openness, responsibility, and involvement. They use quantifiable results to gauge development. It is essential to evaluate and thoroughly modify methods based on proof. In general, based on information focused on community management promotes equality, focuses efforts forward, and addresses the structural causes of obesity in various groups (Centers for Disease Control and Prevention, 2019).
Environmental and Epidemiological Data
In the US, obesity is a serious public health concern. Key findings from recent national surveys (CDC, 2022; Food et al. Center, 2020; National Institute of Diabetes and Digestive and Kidney Diseases, 2021) on the overall incidence of overweight and obesity amongst Americans of all ages are shown in the data table as follows:
Table 1: Statistical data on obesity in the United States
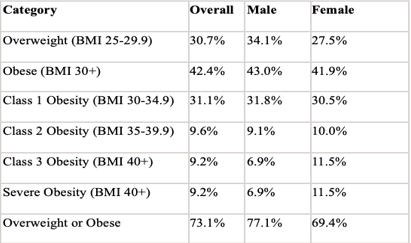
Approximately 3 out of 4 individuals in the United States are overweight or obese (73.1%), according to the statistics in the table, which shows unacceptably high proportions of these conditions across adult Americans. There is a noticeable increase in the incidence of obesity in particular categories, such as men vs women in overweight (34.1% vs. 27.5%) and women versus men for serious weight gain (11.5% vs. 6.9%) (CDC, 2022). According to these figures, overweight is a serious public health concern that requires immediate response. External factors, such as limited availability of nutrient-dense meals, insufficient resources for physical exercise, or obesogenic architectural landscapes in many places, mostly cause increased numbers of obese people. The information is derived from the most current findings of the Food Research and Action Center (2020), which provide highly accurate and reliable, broadly representative standard metrics. The report emphasizes how severe the crisis of obesity is and how proven remedies are needed, with a focus on inequalities that primarily affect disadvantaged demographic categories (CDC, 2019).
Ethical Health Improvement Plan
Contextual constraints like restricted access to nutrient-dense meals and a shortage of secure parks or playgrounds should be taken into consideration in any ethical health enhancement strategy aimed at reducing obesity. Along with high levels of crime, it has to address how inequality limits access to healthy options and discourages exercising outdoors. In order to empower vulnerable populations and bring about real improvements, these obstacles must be sensitively overcome. Minorities are particularly affected by these barriers, which exacerbate inequality (Wolfenden et al., 2020).
A focused strategy with quantifiable results is essential for ethically addressing obesity. Initially, in order to improve the accessibility of reasonably priced, healthful food alternatives, authorities should provide financing and opportunities for convenience stores to develop in marginalized communities. High-risk groups need to be covered by medical plans for diabetes tests and counseling regarding nutrition. Schools need to restrict access to nutritious foods and beverages and develop strong exercise programs. Governments at the local level must increase the number of secure outdoor recreation areas in areas of low income. Together, these groups of people may take concerted action to lower the overweight and obesity rate, especially for the most disadvantaged. Quantifiable decreases should be tracked to show moral success against the current health crisis. To encourage nutritious habits while honoring dietary practices, appropriately culturally sensitive outreach and training are required (Platter et al., 2021).
Reductions in BMI and instances of obesity among high-risk groups must be measured as a success criterion. Surveys must nevertheless also monitor better medical habits and expanded possibilities for fitness and dietary options. To direct future attempts and legislative adjustments, data collecting ought to reveal any gaps that still exist. A moral strategy may modify the growing obesity epidemic sloped with coordinated, sympathetic initiatives that concentrate on the ones who are affected. It is equally vital that these programs encourage populations to drive remedies while hospitals and clinics provide proper wellness services and rehabilitation for obesity (Lappan et al., 2020).
Intervention, Barriers, and Evaluation Criteria
Multilevel treatments that enhance both diet and exercise in high-risk groups are necessary to reduce obesity. Using culturally relevant teaching, expanding the availability of reasonably priced products, and providing safe recreational areas, advertisements may encourage modifications to the behavior (Wolfenden et al., 2020). Particular obstacles, such as dietary customs or security concerns, must be addressed cautiously, nevertheless. Achievement should be measured by a lower BMI, especially for ethnic minorities. However, important factors like rates of involvement, how well resources are used, and healthy habits are also important. To help guide further attempts, questionnaires and feedback from the community may supplement numerical information (Platter et al., 2021).
NURS FPX 6011 Assessment 2 Evidence Based Population Health Improvement Plan
It is also important to assess the achievement made toward systems-change objectives such as improved educational meals, broader public transportation, more extensive coverage through insurance for dietary offerings, and permitting regulations that support living an active life. Such changes in our surroundings are necessary to have a long-lasting effect on overweight. Following them reveals that significant shift often happens gradually. We may objectively measure the effect and drive policy to attain health equality by addressing adiposity throughout all groups using community-centered standards to track health consequences and generate variables (Kitson et al., 2021).
Implementation of Population Health Improvement Plan
Collaborations with neighborhood groups that support those in need, such as the Obesity Action Coalition (OAC), are going to be essential to carrying out an obesity management strategy responsibly and efficiently (Obesity Action Coalition, 2019). Food stores, educational institutions, parks agencies, transportation leaders, religious organizations, and neighborhood health clinics are examples of pertinent stakeholders. It will be crucial to communicate with respect and develop trust. Sessions need to take into account cultural norms, difficulties with medical education, and worries about the confidentiality of information (Platter et al., 2021). Accessibility will be improved by providing medical ideas in a straightforward manner and by using anonymized or aggregated information. Comment may be gathered, and news about progress can be shared via brochures, television shows, institutions of learning, and congregations, among various other methods (Vaughan et al., 2021).
One way to politely share views and observations with nonprofit organizations is to organize a neighborhood advisory board with members drawn from the affected populations. This demographic may direct the right message and customization of interventions. Collaborating with Latino congregations, for instance, might provide invaluable insights into communicating nutrition principles in a manner that is both relevant and respectful of ethnic culinary customs. It will be crucial to maintain constant contact via discussion forums, consultative committees, and open community gatherings. This will guarantee that the strategy takes care of the underlying causes of overweight or obesity, which include injustice toward the environment, impoverishment, hazardous communities, and an absence of access to preventative treatment. Not only is the interaction that promotes the exchange of knowledge moral, but it is also practical. For the purpose of developing long-lasting solutions to challenging safety issues, the firsthand knowledge of community members is essential (Calancie et al., 2023).
Value and Relevance of Evidence
For the purpose of setting objectives and monitoring advancement over time, precise, up-to-date statistics on the prevalence of obesity are crucial. Important statistical information showing rising instances of overweight over the last 20 years, particularly severe weight gain, may be found in the NIDDK (2021) numbers. Population breakdowns highlight inequalities that need to be addressed; for example, certain classes of obesity have a greater prevalence of overweight among men and women and racial minorities. The use of sophisticated mapping and information analysis programs may help guide initiatives to avoid obesity. Geographical investigation, for instance, may be used to determine “food deserts” and workout deficiencies in infrastructure in local areas. Algorithms for predictions may also be used to assist resource allocation by estimating future illness prevalence and expenditures under multiple intervention possibilities (Buchanan et al., 2020).
Studies clarifying the environmental causes of obesity are also very important, especially for underprivileged groups. According to research by Blackstone and Herrmann (2020), obesity is mostly caused by low-income areas’ poor exercise opportunities and restricted access to wholesome, reasonably priced meals. This emphasizes how important it is to modify policies and implement focused initiatives to increase the utilization of healthy nutrition and physical activity in underprivileged communities.
Specific Actions of Community Stakeholders
To pull alongside various organizations in the community to promote significant change, seamless interaction will prove essential. The purpose of the first sessions should be to present scientifically supported strategies and get opinions on their viability and suitability for the community at large. It will be easier to adapt projects so that they align with the objectives and values of organizations if thorough listening and transparent communication are encouraged. Occasional advancement reports using chosen methods for communication, such as conversations, newsletters by email, online platforms, and religious announcements, may maintain openness on continuing necessities and problems and foster prolonged involvement by celebrating modest victories (Leuchtag et al., 2022).
Participants ought to be encouraged to demonstrate effort according to their areas of competence in order to promote true ownership. Neighborhood grocery stores may start offering nutrition instruction in-store, for example. Menus at dining establishments may provide more healthful selections. Schools might implement recess rules. Faith-based organizations could organize cooking lessons or strolling organizations that include various ethnic foods. Fresh vegetables might be increased at homeless shelters and banks. These community-based volunteer initiatives have enormous potential to modify social expectations and support more significant changes in governments (Platter et al., 2021). In order to build groups, messaging must remain diplomatic, but consumers must also feel like active contributors to the resolution as opposed to just receivers of an outside strategy. Their judgment and deeds are crucial in converting data into practical effects (CDC, 2019).
Conclusion
Although weight gain is a major threat to the public’s health, it is a complicated problem with many different aspects that need to be addressed in different settings. Targets and actions to support healthy lives may be determined via a data-driven organizing approach for health enhancement. However, real change necessitates identifying and removing the particular obstacles that disadvantaged populations experience. The key to success is a compassionate discourse that builds community involvement and involves a variety of participants. Though it can seem slow, little victories can gather steam. It is possible to slow down the growing problem of obesity by implementing evidence-based interventions via comprehensive cooperation, provided that there is a persistent and unifying vision of health equality. Communities come along at the start of the process to turn ideas into practice.
References
Blackstone, S., & Herrmann, L. (2020). Physical activity among low-income food pantry patrons: Improving the role of a rural food pantry. American Journal of Health Studies, 29(3).
https://doi.org/10.47779/ajhs.2014.223
Buchanan, C., Howitt, M. L., Wilson, R., Booth, R. G., Risling, T., & Bamford, M. (2020). Nursing in the age of artificial intelligence: Protocol for a scoping review. Journal of Medical Internet Research Research Protocols, 9(4).
Calancie, L., Fair, M. L., Wills, S., Werner, K., Appel, J. M., Moore, T. R., Hennessy, E., & Economos, C. D. (2023). Implementing a stakeholder-driven community diffusion-informed intervention to create healthier, more equitable systems: A community case study in Greenville County, South Carolina. Frontiers in Public Health, 11.
https://doi.org/10.3389/fpubh.2023.1034611
CDC. (2019). CDC – Assessment – Community health assessment – STLT Gateway. Centers for Disease Control and Prevention.
https://www.cdc.gov/publichealthgateway/cha/assessment.html
CDC. (2022, May 17). Adult obesity facts. Centers for Disease Control and Prevention.
https://www.cdc.gov/obesity/data/adult.html
Centers for Disease Control and Prevention. (2019). CDC – Assessment and plans – Community health assessment – STLT Gateway. CDC.gov.
https://www.cdc.gov/publichealthgateway/cha/plan.html
Food Research and Action Center. (2020). Obesity in the U.S. Food Research & Action Center.
https://frac.org/obesity-health/obesity-u-s-2
Kitson, A. L., Harvey, G., Gifford, W., Hunter, S. C., Kelly, J., Cummings, G. G., Ehrenberg, A., Kislov, R., Pettersson, L., Wallin, L., & Wilson, P. (2021). How nursing leaders promote evidence‐based practice implementation at point‐of‐care: A four‐country exploratory study. Journal of Advanced Nursing, 77(5), 2447-2457.
https://doi.org/10.1111/jan.14773
Lappan, S. N., Carolan, M., Parra-Cardona, J. R., & Weatherspoon, L. (2020). Promoting healthy eating and regular physical activity in low-income families through family-centered programs: Implications for practice. The Journal of Primary Prevention, 41(6), 503–528.
https://doi.org/10.1007/s10935-020-00612-1
Leuchtag, A., Bressler, L., Banks, A., & Skinner, D. (2022). The importance of communication in collaborative community development: Lessons learned from three cases. Ohio Journal of Public Health, 5(1), 13–19.
https://doi.org/10.18061/ojph.v5i1.8721
NIDDK. (2021, September). Overweight & Obesity Statistics | NIDDK. National Institute of Diabetes and Digestive and Kidney Diseases.
Obesity Action Coalition. (2019). Obesity Action Coalition. Obesity Action Coalition.
https://www.obesityaction.org/
Platter, H., Kaplow, K., & Baur, C. (2021). The value of community health literacy assessments: Health literacy in Maryland. Public Health Reports, 137(3), 471-478.
https://doi.org/10.1177/00333549211002767
Vaughan, J. G., Victora, C. G., & Chowdhury, R. (2021). Communicating health information. Oxford University Press EBooks, 171–177.
https://doi.org/10.1093/med/9780192848741.003.0013
Wolfenden, L., Williams, C. M., Kingsland, M., Yoong, S. L., Nathan, N., Sutherland, R., & Wiggers, J. (2020). Improving the impact of public health service delivery and research: A decision tree to aid evidence‐based public health practice and research. Australian and New Zealand Journal of Public Health, 44(5), 331-332.
https://doi.org/10.1111/1753-6405.13023
Get more information about this MSN flexpath assessments click below to view:
NURS FPX 6025 Assessment 3 Practicum and Scholarly Article