- BHA FPX 4110 Assessment 1 Vila Health Patient Flow.
Vila Health Patient Flow
Providing great healthcare to individuals is the primary target of every healthcare business. The organization must advance and encourage collaboration among healthcare experts of all specialties to achieve this goal. Furthermore, healthcare workers must be prepared to offer great assistance with minimal or no errors. Cultural ability, compassion, kindness, and honesty all add to the quality of care that can be given. Patients will get better quality care if a hospital has a more significant level of these factors.
In addition, patients are happier when they get better healthcare services in a facility of better quality. As a result, the institution sees an increase in patient traffic. In a request to fix the issue of low patient satisfaction at Vila Health, several problems have been addressed.
Why patient satisfaction is so important in the healthcare industry
From a financial standpoint, patient happiness is one of the most important parts of a healthcare institution (Ng & Luk, 2019). Patient satisfaction is the greatest way to measure and evaluate the quality of healthcare services in a healthcare facility. Patients will return to a facility if they are satisfied with the treatment level, which is a natural result of improving the hospital’s quality of service delivery. Why? Because superb service attracts patients who will indeed return to the facility again. The more patients an institution accepts, the more cash it makes. In the healthcare industry, patient happiness acts as a strategic position. Most facilities strive to deal with patient happiness to gain a strategic position, but those who succeed also gain a larger percentage of income.
The Independence Medical Center (IMC) considers patient satisfaction a strategic effort because of its vital position in the hospital. The facility’s patient satisfaction ratings have been a valuable tool in identifying areas for improvement, as discussed in the BHA FPX 4110 Assessment 1 Vila Health Patient Flow. The gadget serves as an intermediary for evaluating the quality of care and ideal service conveyance and assessing the effectiveness of providing care services to patients (Ng & Luk, 2019). Surveys of patients have been used to gauge the level of satisfaction with the facility’s services, and the results have assisted the facility with identifying areas that need improvement as well as parts that are doing great and should be preserved.
Initiative for Improving Results
Healthcare facilities use performance improvement initiatives to discover and assess the gaps in healthcare delivery and address them to improve the patient experience. Patient self-management techniques that foster treatment results are being created and tested as part of this program, incorporating behavioral changes and healthcare systems. Aside from that, the vital aims of the organization are formulated, and the results of implementing the system changes are seen. Indeed, the primary target of all the activities carried out is to enhance the conveyance of healthcare services.
- Improving Patient Satisfaction Challenges
IMC’s practices show that patient happiness is one of the most compelling ways to foster healthcare services further. Elevated degrees of patient satisfaction suggest healthier lifestyles in the surrounding areas. A decline in patient satisfaction could incite the IMC’s leaders to consider a further facility push to foster performance. The facility’s executives can better understand areas that require additional resources and contribute scarcely anything to patient satisfaction through such an initiative.
To ensure patient outcomes are dealt with, the facility’s management will want to ask the public authority for help in the form of finances, gear, and additional staff members. Unfortunately, communication between healthcare providers is one of the major contributors to the facility’s deteriorating patient satisfaction, according to data acquired from IMC. In addition, the number of healthcare practitioners, particularly medical doctors, is exceptionally low relative to the number of patients served. As a result, patients’ frustration grows as the waiting time lengthens. Because of the significant delays, patients cannot move between units expeditiously, resulting in unfortunate patient care.
Anatomy of a Fishbone
Visual representations of a fish’s bones can be used to distinguish the fundamental causes of an issue and feature its drawn-out implications. On the right side of the fishbone, representing the conclusion is an issue that must be handled. While drawing a fishbone diagram, you will see subcategories labeled as a branch of the main bone. Nonetheless, several ‘why’ questions must be addressed to speed up the work on the issue.
The first step in determining the issue’s main categories is to list all the components that should be addressed. Problems inside an organization must be acknowledged for its features to be known. After carefully surveying all the relevant factors, possible solutions are gathered to determine the best course of action. At the point when the best solution has been determined, the stakeholders concerned archive their agreement. Contingencies are designed, checked, and investigated to meet the desired result. As outlined in the stakeholders’ fishbone graphic, the methodology must be followed step-by-step.
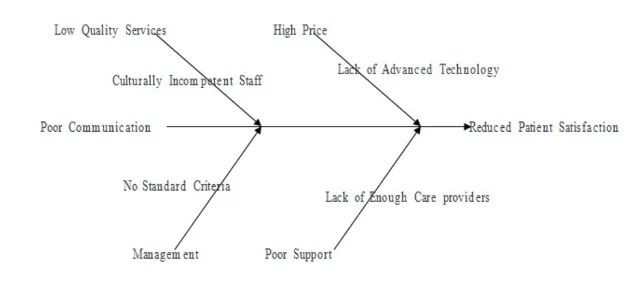
The head of the fishbone diagram is based on the main pressing concern: diminished patient satisfaction. High pricing and weak support are found in the first subcategory pair. ” The significant expense of innovation makes it hard to execute, while the shortage of healthcare providers results in unfortunate support. Higher on this scale reflects unfortunate service, whereas lower is managerial quality. Culturally unskilled healthcare workers are to blame for unfortunate service quality, while management has not established a standard service model.
A Performance Improvement Team’s Purpose
A performance improvement team must be included because of their vital role in achieving the organization’s goals. The team’s cooperation helps determine the best way to deal with the issue seen in the organization. Team members cooperate to think of innovative solutions that address the underlying drivers of the main problem. Assigning tasks, scheduling meetings, and allocating resources are all responsibilities of the performance improvement team. The team includes members of the organization’s personnel, including managers, facilitators, and other leaders, such as supervisors. The facility must have representatives from several professions, such as doctors, pharmacists, and nurses.
All relevant information from various professions and departments will be made available to the facility’s critical thinking team as required. Patients should also have a representative in the performance improvement team. This is because patients represent a significant part of the facility’s stakeholders.
Methodology of Lean
A business strategy ensures continual improvement in client service delivery using lean principles (Karaca & Durna, 2019). Reducing patient wait times and lobbying for better healthcare conveyance are two goals of the lean healthcare idea. In addition, the strategy helps find patient value, construct a flow, map the value stream, develop a draw, and create an ideal pattern. DMAIC and manufacturing initiatives are examples of projects that take advantage of lean methodology.
Model of DMAIC
The acronym DMAIC stands for “define, measure, analyze, improve, and control” an organization’s operations (Rana & Kaushik, 2018). DMAIC is included in the Lean Six Sigma framework as part of a quality improvement program. The model is most used during critical thinking processes to increase a company’s performance. The undertaking managers begin by defining the purpose and scope of the work. Value improvement processes are also outlined. The critical thinking strategy is seen, and data is gathered to start the analytic phase. For further investigation, this helps to discover what is causing the issue. Additional study is required to ensure the problem is solved and regulated.
Patient dissatisfaction has been seen as the primary issue at Vila Health. Several factors add to the problem, but the most significant is a lack of coordination among healthcare providers. Patients’ health deteriorates due to substantial delays caused by a Shortage of medical personnel in the facility. Patient unhappiness arises due to this (Rana & Kaushik, 2018). This issue necessitates collecting data from patients and healthcare experts to determine the underlying cause.
- Addressing Patient Satisfaction Issues
The facility’s patient satisfaction rating, treatment conveyance proficiency, and post-service results are all important information to have on hand. Ineffective communication, a lack of care providers, a lack of funding to address the facility’s issues, and a lack of patient involvement in care conveyance are the most notable underlying drivers of poor patient satisfaction.
The organization’s stakeholders must cooperate to solve the challenge, as outlined in the BHA FPX 4110 Assessment 1 Vila Health Patient Flow. To solve problems, the chosen performance improvement team must upgrade the usage of numerous techniques, such as considering lean methodology, the DMAIC model, and the thesis sigma strategy. The major issue of low patient satisfaction can be addressed by addressing the underlying causes revealed through these strategies. Medical experts, moreover, the public authority must also provide technological devices associated with innovation to foster care delivery proficiency.
References
Karaca, A., & Durna, Z. (2019). Patient satisfaction with the quality of nursing care. Nursing Open, 6(2), 535-545. https://doi.org/10.1002/nop2.237
Ng, J. H., & Luk, B. H. (2019). Patient satisfaction: Concept analysis in the healthcare context. Patient education and cocounseling102(4), 790-796. https://doi.org/10.1016/j.pec.2018.11.013
Rana, P., & Kaushik, P. (2018). Six-sigma derivatives: A case study. Management Science Letters, 8(8), 849-858. 10.5267/j.msl.2018.6.003

